Prednisone is not a casual medication. It has helped millions manage chronic inflammation, survive allergic reactions, and recover from autoimmune flares. But it demands respect. Understanding how it works, managing its side effects, and working with a healthcare provider are key to using it safely.
Prednisone Corticosteroid Prices
Prednisone 40 mg –> from $ 0.42/pill
Prednisone 20 mg –> from $ 0.36/pill
Prednisone
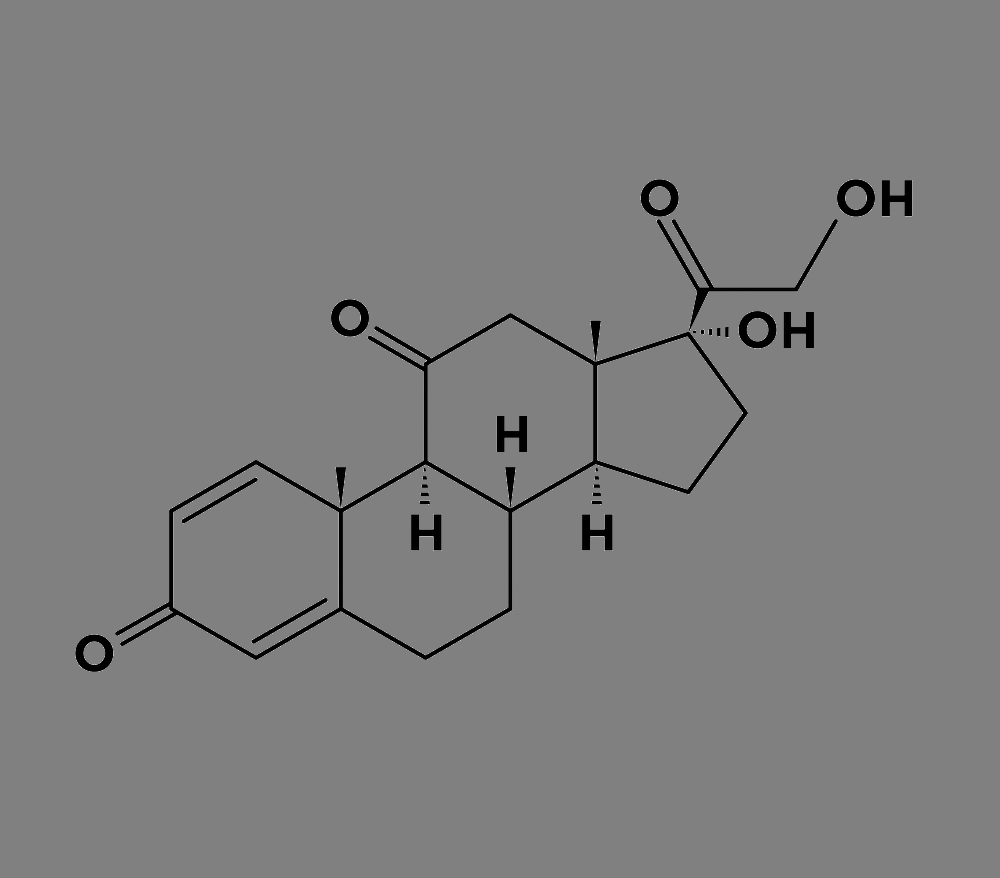
Prednisone is a synthetic corticosteroid drug commonly used to treat inflammation and suppress the immune system. It mimics the effects of cortisol, a natural hormone produced by the adrenal glands. Due to its broad impact on multiple body systems, prednisone is used to manage a wide range of conditions—from autoimmune diseases to allergic reactions and chronic respiratory issues.
What Is Prednisone?
Prednisone belongs to a class of drugs known as glucocorticoids. These drugs reduce inflammation and affect the immune response. After oral administration, prednisone is converted by the liver into prednisolone, its active form.
Key Facts
- Drug class: Corticosteroid
- Common brand names: Deltasone, Rayos
- Routes of administration: Oral tablets, liquid
- Prescription required: Yes
- Half-life: 2 to 4 hours (biological effects can last longer)
What Are Corticosteroids?
Corticosteroids are synthetic drugs designed to mimic cortisol, a hormone produced by the adrenal glands. They come in two main types: glucocorticoids and mineralocorticoids. Prednisone falls under glucocorticoids, which primarily reduce inflammation and suppress the immune system. These drugs are widely used to treat autoimmune conditions, allergies, asthma, and more. While highly effective, corticosteroids must be used carefully due to their potential side effects, especially with long-term use.
What Does Prednisone Treat?
Prednisone is prescribed for short-term and long-term use depending on the condition. It's not a cure, but it helps control symptoms and reduce flare-ups.
Common Conditions Treated with Prednisone
| Category | Conditions |
|---|---|
| Autoimmune diseases | Rheumatoid arthritis, lupus, vasculitis |
| Respiratory issues | Asthma, COPD exacerbations |
| Skin disorders | Psoriasis, eczema, dermatitis |
| Allergic reactions | Severe allergic reactions, hives, anaphylaxis support |
| Blood disorders | Anemia, thrombocytopenia |
| Neurological | Multiple sclerosis flares |
| Gastrointestinal | Crohn’s disease, ulcerative colitis |
| Cancer support | Part of chemotherapy regimens to reduce inflammation |
| Organ transplants | To prevent rejection |
How Prednisone Works
- Inhibiting inflammatory pathways.
- Reducing the production of substances that trigger allergic and immune responses (e.g., prostaglandins, cytokines).
- Decreasing white blood cell activity.
Dosage and Administration
Prednisone is available in various strengths. The dose depends on the condition, severity, and patient response.
General Dosage Guidelines
- Low dose: 5–10 mg/day – often for chronic conditions
- Moderate dose: 10–40 mg/day – flares or acute treatment
- High dose: 40–100+ mg/day – severe cases like organ rejection or acute inflammation
It’s usually taken once daily in the morning to align with natural cortisol cycles.
Is Prednisone Available Over the Counter?
No, prednisone is not available over the counter in most countries, including the United States. It requires a prescription because of its powerful effects on the body and its potential for serious side effects. Self-medicating with prednisone is unsafe. Even short courses should be supervised by a healthcare provider, who can assess whether the benefits outweigh the risks and monitor for complications. If you're experiencing symptoms that might require prednisone, it's best to consult a doctor rather than trying to find it through non-prescription means.
Common Side Effects
Short-Term Side Effects
- Increased appetite
- Insomnia
- Mood swings
- Fluid retention
- Stomach upset
Long-Term Side Effects
| System Affected | Potential Effects |
|---|---|
| Musculoskeletal | Osteoporosis, muscle weakness |
| Metabolic | Weight gain, diabetes, high blood sugar |
| Cardiovascular | High blood pressure, increased risk of heart disease |
| Dermatological | Acne, thinning skin, slow wound healing |
| Ocular | Cataracts, glaucoma |
| Endocrine | Adrenal suppression, Cushing’s syndrome |
| Immune | Increased infection risk |
| Psychological | Depression, euphoria, psychosis |
Cautions and Warnings
- Adrenal Suppression: Long-term use suppresses natural cortisol production. Stopping suddenly can be dangerous.
- Infection Risk: The immune system is weakened.
- Bone Health: Reduced density; supplements are often needed.
- Blood Sugar: Can raise glucose levels, especially in diabetics.
Prednisone Tapering
You can't stop prednisone abruptly after long-term use. Tapering is essential.
Typical Tapering Strategy
- Reduce dose by 10–20% every 1–2 weeks
- Watch for withdrawal symptoms: fatigue, aches, dizziness
- Adjust based on how the body reacts
Drug Interactions
- NSAIDs: Higher ulcer risk
- Diuretics: Can disrupt electrolytes
- Vaccines: Live vaccines are not recommended
- Antifungals: May increase steroid levels
- Blood thinners: Effect can vary, needs monitoring
Prednisone in Special Populations
Children
Used cautiously due to growth suppression risks. Doses are weight-adjusted.
Pregnant Women
Only when necessary. Prednisone crosses the placenta but is metabolized quickly.
Elderly
More sensitive to side effects. Lower doses and bone protection may be needed.
Lifestyle and Monitoring Tips
- Diet: Low sodium, high potassium, calcium, and vitamin D
- Exercise: Weight-bearing to preserve bone
- Sleep hygiene: Manage insomnia risk
- Regular checkups: Blood sugar, bone scans, eye exams
Alternatives to Prednisone
| Condition | Alternatives |
|---|---|
| Rheumatoid arthritis | Methotrexate, biologics |
| Asthma | Inhaled corticosteroids, leukotriene modifiers |
| Lupus | Hydroxychloroquine, immunosuppressants |
| Inflammatory bowel disease | Mesalamine, biologics |
Misconceptions About Prednisone
- "It’s just a strong painkiller." False. It reduces inflammation, not pain directly.
- "You’ll always gain weight." Not necessarily. Managed with diet and dose.
- "It works instantly." It may take a few days to show full effect.
Real-World Use Cases
Case 1: Asthma Flare-Up
Short course of 40 mg/day brings rapid relief by Day 2.
Case 2: Lupus
Maintenance dose of 7.5 mg/day keeps flares in check with regular bone monitoring.
Case 3: Transplant Patient
Used as part of immunosuppressive therapy, tapered to 5 mg/day over time.
Key Takeaways
- Effective anti-inflammatory and immune suppressant
- Short-term use is safer; long-term use needs caution
- Requires tapering and monitoring
- Smart lifestyle choices can reduce risks
Patient Checklist
- ✅ Follow your prescribed dose and timing
- ✅ Don’t stop suddenly without a doctor’s plan
- ✅ Monitor blood pressure, blood sugar, and weight
- ✅ Take calcium and vitamin D if advised
- ✅ Report any signs of infection right away
- ✅ Ask about bone scans if on long-term treatment
- ✅ Keep a list of medications to avoid interactions

